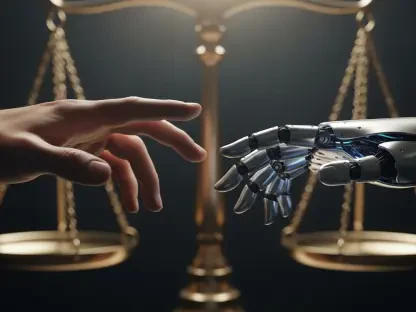
Telemedicine has seen unprecedented growth, especially during the pandemic. However, navigating the complex legal and regulatory landscape remains a significant challenge. This article explores pivotal telemedicine policy trends, legal hurdles, and strategies to enhance telehealth practices in the face of these challenges.
The Rise of Telemedicine and Its Post-Pandemic Landscape
Telemedicine experienced rapid growth during the COVID-19 pandemic, highlighting its potential to transform healthcare delivery. As the pandemic wanes, the regulatory environment has evolved, presenting new challenges that require careful navigation.
The Impact of the Public Health Emergency
One notable change is the end of the Public Health Emergency (PHE) on May 11, 2023. This event marked the beginning of a new era for telemedicine policy, leading to debates and updates by key federal players such as the DEA and Congress on telehealth practices. The end of the PHE signaled the need for comprehensive approaches to sustain telemedicine’s growth and address emerging legal and regulatory complexities. The significant expansion of telehealth services during the pandemic necessitated new compliance measures and adjustments to existing policies to ensure continuity and quality of care.
Amid these developments, the DEA and Congress took proactive steps to address the evolving telehealth landscape. The DEA extended certain prescribing waivers, acknowledging the critical role telemedicine played in patient access to essential treatments. Concurrently, Congress introduced legislative initiatives aimed at extending Medicare flexibilities, underscoring the importance of crafting regulatory frameworks that not only support telehealth continuity but also enhance the scalability and scope of services delivered via telemedicine.
Legislative Adaptations
From 2024 to 2025, significant legislative efforts aimed to extend Medicare flexibilities and refine telehealth policies, underscoring the need for forward-thinking regulatory frameworks that sustain the telemedicine advancement achieved during the pandemic. Legislative bodies recognized the pressing need to bolster telemedicine infrastructure, mitigate administrative hurdles, and provide clear guidelines for telehealth practices. During this era, legislative measures were instrumental in streamlining the compliance landscape, fostering a conducive environment for both patients and clinicians.
These legislative adaptations focused on several key areas to enhance telehealth accessibility and effectiveness. Policy refinements were designed to address lingering ambiguities in telemedicine regulations, promote greater consistency in enforcement, and encourage the use of technology in healthcare delivery. By leveraging insights gained during the pandemic, lawmakers worked to enshrine telehealth advancements into law, ensuring their benefits were sustained beyond the immediate crisis and integrated into regular healthcare practices.
Key Legal and Compliance Challenges
Telemedicine continues to face several legal and compliance challenges that impede its widespread adoption and efficient implementation.
Privacy and Security Concerns
A major concern in telemedicine is the privacy and security of patient information. While clinicians must use HIPAA-compliant platforms post-PHE, issues persist, particularly with third-party applications, raising significant concerns about data protection in mental health services. The sensitive nature of health information, especially in mental health contexts, necessitates robust security measures to prevent unauthorized access and breaches.
Providers are often caught in a precarious position, balancing the need for accessible and efficient telehealth services with the stringent requirements of data privacy laws. Ensuring patient confidentiality while using interoperable platforms involves continuous monitoring, compliance audits, and the use of encrypted communication channels. Despite these efforts, the complexity of maintaining comprehensive cybersecurity protocols means that lapses can and do occur, potentially eroding patient trust and compliance.
Interstate Practice and Licensure
Licensing requirements across states present another barrier to telemedicine. Although initiatives like the Medical Licensure Compact and Nurse Licensure Compact aim to streamline licensing, variations in state standards complicate interstate telehealth practices. Each state retains the authority to set its own licensure criteria, creating a mosaic of regulations that can be difficult for practitioners to navigate, especially those seeking to offer services across multiple states.
These regulatory differences necessitate that healthcare providers become well-versed in the legal standards of each state in which they practice, increase administrative burdens, and introduce potential delays in care. Furthermore, telehealth practitioners may encounter challenges in reimbursing services from payers who also have to account for state-specific regulations. These intricacies highlight the need for more uniform regulatory approaches to facilitate the seamless practice of telemedicine across state lines.
Prescribing Regulations
Policies on prescribing over telemedicine, such as the DEA’s final rule on buprenorphine prescribing, continue to evolve. These regulations have critical implications for access to treatments, especially for substance use disorders, and impact interstate licensure. The ability to prescribe controlled substances via telemedicine has been a significant advancement, offering a lifeline to patients in need of immediate care. However, achieving a balance between leniency for patient access and rigorous oversight to prevent misuse remains a challenging endeavor.
The regulatory framework governing telemedicine-prescribing practices depends on precise guidelines and effective enforcement mechanisms. This includes meticulous tracking of prescribing patterns and regular updating of protocols to reflect current best practices and emerging threats. For healthcare providers, staying compliant with evolving prescriptions requires continuous education and adaptation, while ensuring that patients receive timely and appropriate care.
Recommendations for Enhancing Telemedicine Practices
Building on the identified challenges, this section provides recommendations for improving telemedicine accessibility and effectiveness.
Simplifying Policies
Reducing administrative burdens through simplified and clear policies can particularly benefit smaller practices with limited resources. This approach aims to make compliance more manageable and foster the wider adoption of telemedicine. Simplified guidelines enable healthcare providers to focus more on patient care rather than navigating the legal maze, facilitating smoother operations and enhanced service delivery. Additionally, making policies more transparent and understandable can reduce the risk of unintentional non-compliance and promote higher standards of care.
Small practices, often constrained by limited staff and financial resources, can particularly benefit from streamlined administrative protocols. These groups may struggle to keep up with the complex requirements, and thus, policy simplification can alleviate the burden, enabling these practices to integrate telemedicine more effectively into their services. This, in turn, extends the reach of telehealth solutions to more patients, particularly those in underserved areas.
Enhancing Privacy and Security
Strengthening protocols for protecting patient information is vital. The adoption of advanced technologies and stringent security measures can mitigate privacy concerns and build trust among patients and providers. Technologies like end-to-end encryption, biometric authentication, and secure cloud storage can provide robust defenses against data breaches and unauthorized access. Incorporating Artificial Intelligence (AI) for continuous monitoring and threat detection can also add an additional layer of security.
Healthcare providers must prioritize regular training and updates for their staff on the latest privacy practices and compliance requirements. High standards of communication between technical and medical staff ensure that security measures are effectively implemented without compromising patient care. Building a culture that emphasizes data privacy enhances both compliance and patient assurance in the security of their telehealth interactions.
Facilitating Interstate Telemedicine Practice
Further developing interstate licensure compacts and uniform standards will reduce barriers for providers, allowing for seamless telemedicine practice across multiple states and enhancing patient access to diverse healthcare services. Simplifying the licensure process through widely accepted compacts or a national standard can reduce the administrative burden on clinicians, promoting a more dynamic and responsive telehealth environment.
By creating a cohesive regulatory framework that is recognized across states, providers can offer their services to a wider patient demographic without constantly adapting to different legal requirements. This can improve the quality of care, lower costs, and increase patient access to specialized treatments that may not be available locally. National and state regulatory agencies need to collaborate on establishing these uniform standards to ensure consistency and interoperability throughout the healthcare network.
Clarifying Prescribing Guidelines
Establishing consistent guidelines for telemedicine prescribing, informed by comprehensive research, will promote standardized practices and ensure compliance, benefiting both clinicians and patients. Clear regulatory frameworks for prescribing practices reduce ambiguity and allow practitioners to make informed decisions that align with legal requirements and clinical best practices. This clarity benefits patients by ensuring they receive timely and appropriate prescriptions without unnecessary delays or administrative hurdles.
Policymakers should leverage data-driven insights to refine prescribing guidelines that consider the unique aspects of telehealth care delivery. Regular updates to regulations, based on emerging evidence and technological advancements, ensure that telemedicine remains a safe and effective method for patient treatment. Institutions can collaborate on developing best practices and standardized protocols for telehealth prescribing, ensuring wide adoption and adherence across the healthcare system.
By addressing these challenges and implementing strategic reforms, the telemedicine field can continue to evolve, providing equitable and efficient healthcare solutions in the digital age.
Embracing the Future of Telemedicine
Telemedicine has experienced incredible growth, particularly during the COVID-19 pandemic. Despite its benefits, the telehealth sector still faces a complex maze of legal and regulatory challenges. This article delves into the key trends in telemedicine policies, the significant legal obstacles the industry encounters, and possible strategies to improve telehealth practices amidst these hurdles. Given the rapid advancements and increasing reliance on digital health services, stakeholders must stay informed and adaptive to navigate this evolving landscape effectively. By understanding and addressing these legal and regulatory complexities, we can better position telemedicine to provide accessible and high-quality care. For patients and providers alike, embracing these enhancements ensures that telemedicine continues to grow and meet the needs of individuals in a constantly changing healthcare environment.