For an alarming number of Americans holding an insurance card, the promise of security has been replaced by the paralyzing fear of a single medical bill that could unravel their financial lives. An extensive and detailed analysis of the evolving landscape of the Affordable Care Act (ACA) reveals a significant and concerning trend: a growing number of Americans are opting for health insurance plans with lower monthly premiums but substantially higher deductibles. This choice, driven by rising costs, may jeopardize their access to necessary medical care and threaten the stability of the insurance marketplace. This consumer shift has emerged as a critical issue within the broader political debate over healthcare affordability, particularly in the lead-up to the midterm congressional elections.
When Affordable Care Comes with an Unaffordable Catch
The Affordable Care Act was designed to provide a safety net, ensuring that millions could access health coverage without fear of being denied for pre-existing conditions. However, the current marketplace presents a sharp paradox. While millions remain insured, a growing contingent finds themselves “functionally uninsured,” holding plans with deductibles so high that seeking routine or even urgent medical care becomes a financially daunting decision. This reality forces a difficult calculation: pay a premium for a plan that might not be usable in a time of need, or risk forgoing insurance altogether.
This predicament is not an accident but the result of shifting economic and political landscapes. The promise of “affordable” care is being tested as consumers are increasingly pushed toward plans that prioritize low monthly payments over accessible, day-to-day healthcare. The central tension is no longer about just being covered, but about the quality and practicality of that coverage when a medical emergency strikes, leaving many families one illness away from potential financial distress.
The Subsidy Cliff and Its Political Fallout
The immediate catalyst for this affordability crisis was the expiration of enhanced federal subsidies on January 1. This legislative change, born from political gridlock, delivered an immediate and severe financial blow to millions of households. According to an analysis by the health research organization KFF, the loss of these subsidies caused annual premiums to spike by an average of more than $1,000 for enrollees who had previously depended on them for financial assistance.
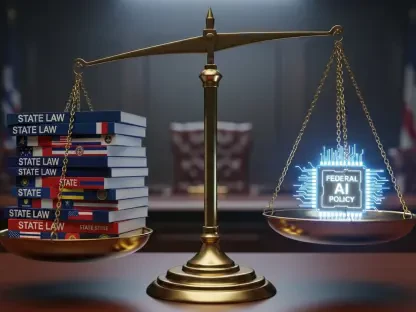
This sharp rise in costs has inevitably become a pivotal battleground in the political arena. Democrats are highlighting the soaring ACA premiums as a key failure of bipartisan cooperation, making it a central theme in their campaign to regain control of Congress. In response, Republicans and the White House are actively promoting alternative solutions aimed at addressing affordability through different mechanisms. The political impasse and its tangible consequences have set the stage for a contentious debate over the future of American healthcare.
The Great Migration to Bronze Plans
The fallout from the premium hikes was immediately visible in enrollment figures. A national snapshot from the Centers for Medicare and Medicaid Services (CMS) showed that ACA signups fell by 1.2 million people, from 24.1 million in 2025 to 22.9 million in 2026. This 5 percent drop was most pronounced on the 30 state exchanges managed by the federal government. Yet, hidden within these numbers is a more subtle and perhaps more consequential trend: a mass migration of consumers from comprehensive coverage to lower-tier “bronze” plans.
This nationwide shift is starkly illustrated by data from several states. In California, despite stable overall enrollment, over one-third of new enrollees chose bronze plans, a dramatic increase from the previous year. Among returning Californians who switched plans, an overwhelming 73 percent moved into a bronze plan. In Maine, these high-deductible plans now constitute nearly 60 percent of all selections. Perhaps most telling is the situation in Rhode Island, where the state exchange witnessed an “explosion” in bronze signups—a 140 percent surge—while enrollment in more robust gold and platinum plans plummeted.
Paying the Price for Lower Premiums
While bronze plans cover the same essential health benefits as their more expensive counterparts, their structure demands that patients bear a much greater share of their medical costs upfront. The critical difference is the deductible, the amount a patient must pay out-of-pocket before insurance begins to cover most services. For the current year, the average individual deductible for a bronze plan is a staggering $7,476, roughly 40 percent higher than the average for a silver plan. For many common medical needs, this entire amount must be paid before any cost-sharing benefits take effect.
This financial barrier can deter individuals from seeking necessary medical care, a concern widely shared among health policy experts. “If you have an expensive health care encounter or expensive illness, you will be responsible for paying that deductible entirely out of pocket,” notes Emma Wager, a senior policy analyst at KFF. This is not just a theoretical risk; it is a documented public health concern. A 2025 study in the Journal of the American Medical Association found that individuals in high-deductible plans were less likely to utilize services for chronic illnesses. Similarly, a 2023 study in Translational Behavioral Medicine concluded that these plans correlated with fewer physician visits, screenings, and vaccinations, even for preventive services that are often covered at no cost.
A Critical Choice for Low-Income Americans
The situation is particularly dire for low-income individuals who face an impossible choice. The ACA includes Cost-Sharing Reductions (CSRs) that can dramatically lower out-of-pocket expenses, but these vital protections are only available to those who purchase a more expensive silver-tier plan. With the expiration of enhanced subsidies, these financially vulnerable enrollees must now choose between a high monthly premium they can barely afford and a dangerously high deductible that could bankrupt them. Last year, 53 percent of all marketplace enrollees utilized CSRs, highlighting the vast number of people now confronting this dilemma.
Potential solutions remain mired in political division. Some bronze plan holders can use Health Savings Accounts (HSAs) to save pre-tax money for medical expenses, but this tool is only effective if it is funded—an unlikely scenario for consumers who chose a lower-tier plan precisely because of financial strain. Republicans have advocated for government-funded HSAs as an alternative to traditional subsidies, but this approach has gained little traction with Democrats, leaving the most vulnerable consumers caught in the middle.
The migration toward high-deductible plans represented a profound shift in how Americans interacted with their health insurance. It moved the public conversation beyond the affordability of monthly premiums to a more urgent question about whether the available coverage provided meaningful access to healthcare. The stability of the ACA marketplaces was called into question, as the trend risked creating an imbalanced risk pool where healthier individuals opted for minimal coverage, leaving sicker, more expensive patients to drive up costs for everyone. Federal and state officials watched these developments closely, understanding that the choices made by millions of individuals under financial pressure had the power to reshape the nation’s healthcare landscape for years to come.