The rapid integration of artificial intelligence into clinical settings promises to redefine medical diagnostics, yet this technological leap forward arrives with a profound question about its fundamental fairness and safety. As algorithms begin to influence life-altering decisions, from identifying disease to guiding treatment, the absence of a comprehensive regulatory framework creates a perilous gap between innovation and patient protection. This report examines the dual nature of AI in healthcare, exploring its transformative potential alongside the urgent need for oversight to ensure that progress does not come at the cost of equity.
The Digital Revolution in Medicine: A Double-Edged Sword
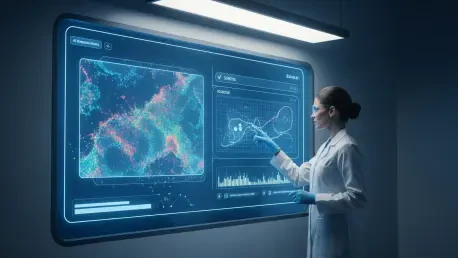
Artificial intelligence is rapidly moving from a theoretical concept to a practical tool within the healthcare landscape, particularly in the field of laboratory medicine. AI-powered systems are being developed to analyze complex datasets from patient samples with a speed and precision that surpasses human capability. This evolution holds the promise of significantly enhanced diagnostic accuracy, streamlined laboratory workflows, and a new era of data-driven clinical decision-making. Key market players, ranging from agile tech startups to established medical device corporations, are fueling this transformation with increasingly sophisticated machine learning models.
However, this wave of innovation carries with it a substantial undercurrent of risk. In an unregulated environment, the very algorithms designed to improve health outcomes can inadvertently cause harm. The performance of these tools is entirely dependent on the data they are trained on, and without standardized validation and verification protocols, there is no guarantee of their safety, efficacy, or impartiality across diverse patient populations. This creates a central conflict where the push for technological advancement outpaces the development of essential safeguards, placing both clinical laboratories and patients in a vulnerable position.
The Momentum of a New Era: AI’s Growth and Impact
Driving the Change: Key Trends in Algorithmic Diagnostics
The adoption of AI in clinical settings is being propelled by a powerful convergence of needs and technological capabilities. A primary market catalyst is the relentless pursuit of greater precision in diagnostics. Healthcare providers and laboratory professionals are increasingly seeking tools that can sift through vast amounts of data to identify subtle patterns indicative of disease, leading to earlier and more accurate diagnoses. This demand for data-driven insight is complemented by the operational need for improved efficiency, as laboratories face mounting pressure to deliver faster results while managing costs.
These drivers are shaping the integration of emerging technologies and influencing professional behaviors. Machine learning algorithms are becoming integral to interpreting complex tests, from genomic sequencing to digital pathology. Consequently, the role of the laboratory professional is evolving from one of pure analysis to one that includes the oversight and validation of these complex computational systems. This shift requires new skill sets and a deeper understanding of data science, marking a significant evolution in the practice of laboratory medicine.
Projecting the Future: Measuring AI’s True Clinical Performance
While financial forecasts for the AI healthcare market point toward exponential growth, a more critical conversation is emerging around how to measure its true value. The focus is shifting from market size to the development of new performance indicators that assess the clinical and societal impact of these technologies. Success can no longer be defined by processing speed or predictive accuracy in a vacuum; it must be measured by demonstrable improvements in patient safety, clinical efficacy, and, most importantly, health equity.
This forward-looking imperative underscores the urgent need to establish standardized benchmarks for validating AI tools. Such standards must ensure that algorithms are rigorously tested in patient populations that reflect real-world diversity, including varied racial and ethnic groups, age ranges, and socioeconomic backgrounds. Without these benchmarks, the industry risks deploying tools that perform well for some but fail catastrophically for others, undermining the ultimate goal of improving healthcare for all.
The Hidden Danger: How Biased Data Creates Unfair Outcomes
The most significant challenge threatening the equitable deployment of AI in healthcare is the risk of algorithmic bias. AI models learn from the data they are given, and if that data reflects existing societal inequities, the resulting tool will not only perpetuate but also amplify those disparities. Many historical medical datasets, which form the training grounds for these algorithms, underrepresent marginalized communities. This creates a critical technological and ethical blind spot.
When an AI system is trained on incomplete or skewed data, its ability to make accurate predictions for underrepresented groups is severely compromised. For instance, a diagnostic tool trained primarily on data from one demographic may systematically misclassify disease or underestimate health risks in others. This can lead to devastating consequences, including delayed diagnoses, incorrect treatments, and a measurable worsening of health disparities. The hidden danger lies in the technology’s ability to codify and scale up human biases under a veneer of objective, data-driven neutrality.
The Regulatory Imperative: Crafting a Framework for Trust and Safety
The growing presence of AI in diagnostics has exposed a significant regulatory vacuum, prompting calls for immediate federal action to establish a framework for trust and safety. Professional organizations are advocating for a multi-pronged approach to oversight, recognizing that existing laws are ill-equipped to handle the complexities of machine learning systems. A key recommendation is the modernization of laboratory regulations, such as the Clinical Laboratory Improvement Amendments (CLIA), to explicitly include standards for the validation, implementation, and ongoing monitoring of AI-driven diagnostic tools.
Central to this new framework is the need for consensus guidelines developed through a partnership between federal agencies and experts in laboratory medicine and informatics. These guidelines would standardize the processes for verifying an algorithm’s performance before it is used in a clinical setting. Furthermore, there is a strong push for initiatives that harmonize laboratory test results and standardize data reporting, which would improve the quality and consistency of the datasets used to train future AI models. Transparency is a cornerstone of this effort, with calls for developers to provide laboratories with the necessary information to independently assess an algorithm’s fairness and accuracy.
Envisioning Tomorrow’s Healthcare: An AI-Powered and Regulated Future
A future where AI is fully and safely integrated into medicine is not only possible but necessary. A robust regulatory framework should be viewed not as a barrier to innovation but as a catalyst for it. By establishing clear rules for safety, efficacy, and equity, regulation can create a trusted environment where developers are encouraged to build responsible and reliable tools. This foundation of trust is essential for widespread adoption by both healthcare providers and patients.
In this envisioned future, laboratory medicine professionals will play an even more critical role as guardians of diagnostic quality. Their expertise will be vital for overseeing the implementation of AI systems, validating their performance against established benchmarks, and ensuring they function as intended within complex clinical workflows. Ultimately, consumer trust will be the final arbiter of AI’s success in healthcare. That trust will be earned through transparent processes, proven fairness, and the demonstrable ability of these technologies to deliver better, more equitable health outcomes for everyone.
The Final Verdict: A Mandate for Equitable Innovation
The deployment of artificial intelligence in healthcare without comprehensive regulation was found to pose an unacceptable threat to patient safety and health equity. While the potential for AI to enhance diagnostics and improve efficiency is undeniable, its capacity to amplify societal biases when trained on unrepresentative data presents a clear and present danger. The core findings of this analysis underscore an urgent mandate for action. Federal agencies, AI developers, and healthcare providers must collaborate to build a future where technological advancement is inextricably linked with justice. This required a concerted effort to modernize laws, establish rigorous validation standards, and demand transparency, ensuring that the next generation of medical innovation serves all patients fairly.